Active listening for powerful impact in health and care
The NHS Constitution states “all staff should have rewarding and worthwhile jobs, with the freedom and confidence to act in the interest of patients. To do this, they need to be trusted, actively listened to and provided with meaningful feedback”.
Yet as we emerge from the pandemic, staff morale and engagement seem to be faltering. Figures from the most recent NHS staff survey indicate that almost a third of respondents think about leaving their organisation, only half of respondents believe that they have a choice in deciding how to do their work, and just half of respondents feel involved in changes being introduced.
Gallup’s long-term research demonstrates how workforce engagement is a critical driver of organisational success. High-engagement organisations outshine their counterparts across various metrics, with 41% better performance in quality, 66% better staff wellbeing, 18% higher productivity, 23% increased profitability, 58% reduction in patient incidents, and an 81% decrease in absenteeism. Yet according to Gallup, a mere 10% of employees in the UK, and 23% of employees worldwide, are classified as engaged.
There is no single solution to solving the challenges facing health and care today. However, staff engagement and empowerment through active listening is an area where every leader can make a meaningful difference. And the cost of not doing this – the cost of inaction – is profound. From more staff leaving, thus increasing pressure on the remaining workforce; to missed opportunities for everyday improvements in frontline operations and care.
This article takes a look at how ImproveWell empowers organisations and teams at a local level to take action. By fostering cultures of active listening and continuous improvement, and enabling leaders to make a demonstrable commitment, the ImproveWell solution puts change-making in the palms of every single member of staff – from ward to board.
THE VALUE AND ROI OF THE IMPROVEWELL SOLUTION
Giving everyone a voice, ImproveWell makes it simple to capture continuous real-time insight from the workforce, improving staff experience and the quality of patient care.
The award-winning solution is grounded in three principles: those at the frontline are best placed to improve the systems around them; giving staff a voice and the agency to find solutions to the challenges they face is fundamental to building a collaborative, motivated and resilient workforce; and a happier workforce leads to better patient outcomes.
Developed in partnership with healthcare organisations and flexible according to local needs, ImproveWell’s evidence-based feedback systems offer a platform for people to drive change, together. Everyone can suggest ideas for improvement, share how their workday is going, and complete tailored pulse surveys – 24/7. Insights from wider stakeholder groups can be gathered and an AI-powered data dashboard enables group and organisational leads to monitor real-time data, track workforce sentiment, prioritise quality improvement efforts, measure change and publish reports to complete the feedback loop.
The value created by implementing the ImproveWell solution within a team or organisation can be summarised as follows:
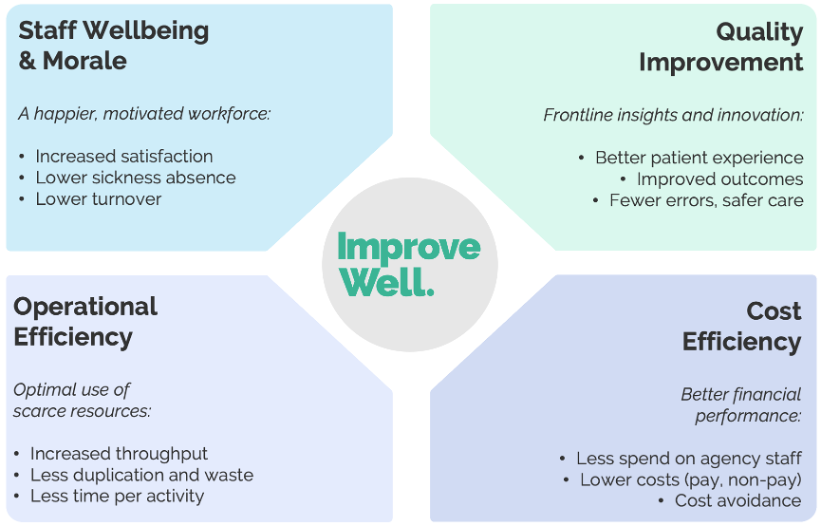
By creating the right environment for workplace wellbeing and continuous improvement through active listening, organisations create:
- Better staff experience – a happier, more motivated workforce leads to higher staff satisfaction, lower sickness absence rates and reduced staff turnover.
- Quality improvement – by leveraging frontline insights and innovation, organisations enhance patient experience, achieve better outcomes and reduce the number of errors or instances of unsafe care.
- Operational efficiencies – optimising the use of scarce resources results in increased throughput, reduced duplication of efforts and improved efficiency.
- Cost savings – improved financial performance results in lower spending on agency staff, reduced costs (both in terms of staff hours saved and waste reduction) and avoided unnecessary expenses.
Our Impact Calculator demonstrates the financial return on investment (ROI) an organisation or team might expect from adopting the ImproveWell solution, in terms of reduced absenteeism, increased retention and the time- and cost-saving improvement ideas gathered and implemented.
Assuming a conservative 0.2% improvement in absenteeism and 0.6% improvement in turnover, a team of 200 and an organisation of 3000 might expect to see savings of £21k and £310k respectively – assuming the starting point NHS national averages of 5% absenteeism (September 2023) and 11% turnover (June 2023).
Savings are not isolated to reduced absenteeism and increased retention. By enabling a constant feed of actionable improvement ideas that often require little or no financial investment, a 200-strong team could expect savings of £91k thanks to financial and time savings, and for a 3000-strong organisation, this figure would be closer to £1.4m.
The ImproveWell dashboard makes tracking impact over time simple. As ideas come in, programme leads can rank improvement ideas according to ease of implementation and impact potential – thus enabling a clear view of where to focus efforts. Ideas can also be categorised by area of impact (e.g. cost savings, time savings, patient safety and experience or staff wellbeing and experience) and yearly cost and time savings can be added to build up a true picture of the solution’s impact over time.
SMALL BUT MIGHTY IDEAS
“ImproveWell was born from the real-world frustration of working in a complex, multi-level organisation and feeling unable to capture, discuss and act on day-to-day moments of inspiration – ‘micro-improvements’ – which, when implemented, deliver compounding benefits of empowering staff and improving patient care.” Dr Na’eem Ahmed, Co-Founder and Chief Medical Officer
Here are some examples of small but mighty ideas submitted by the ImproveWell community to address challenges faced in the day-to-day working environment of frontline staff.
DIGITAL CLOCKS
Inconsistencies in clocks can lead to inconsistencies in administering medicines or treatment; and minutes can make a difference in saving a patient or baby’s life. For example, suppose a baby is distressed at 13:02 and is rushed to the theatre where the clock says 13:06. In such a situation, it becomes difficult to keep an accurate log of any deterioration or improvement in the baby’s condition.
💡Centrally controlled, digital clocks eliminate time-based errors and provide evidence that there are no unaccounted-for delays in care delivery. By implementing the clocks, staff can show there are no unaccounted-for delays in the delivery of care; staff feel more confident in recording timings; and the risk of discrepancies in records and potential litigation is reduced.
TAMPER-PROOF SECURITY TAGS
It is important to ensure that emergency drugs and equipment are routinely checked to ensure they are ready and safe to use when needed. This takes time, and if pressures arise these checks can be missed, leading to safety issues.
💡 Tamper-proof security tags can indicate equipment has been checked and is ready to use. Packs can be checked by breaking the seal at a specified time frequency. The time to check the equipment is reduced, and patient safety is improved. In one ward, a saving in staff time of 22 hours per week has been estimated. This equates to a saving of approximately £19,000 per year, as well as an improvement in patient safety.
AMNESTY BOXES
Staff regularly put things in their pockets during their working day. This can sometimes mean unused medical supplies are accidentally taken home at the end of a shift or left in the changing rooms in the rush to catch a bus, avoid a parking ticket, or get home at the end of a shift.
💡 “Amnesty Boxes” in changing rooms where staff can empty pockets of unused items make it easy for staff to return items and for the unused items to be collected and put back into circulation where possible. For one ward, items returned into circulation have made an estimated saving of around £4,000 per year.
AIR CONDITIONING UNITS
One ward was experiencing an increase in the number of patients developing Acute Kidney Injury (AKI) due to the overwhelming heat and lack of good ventilation on the ward. As well as impacting patient safety, this prolonged the bed stay times, and presented a difficult work environment for staff.
💡 New air conditioning units were installed with additional measures in place for temperature to be monitored regularly. The result was fewer cases of AKI on the ward and reduced bed stays, thus creating cost and time savings. This incremental change generated a better patient experience and, ultimately, a better working environment for the staff.
LASTING, MEASURABLE IMPACT
Everyday improvement ideas and innovation can lead to big impact. The cumulative effect of small, incremental changes can be as powerful as major innovations. As we know from the butterfly effect, shifts in thinking, practice and culture can lead to significant improvements in staff experience and patient care.
Here are some examples of the wider impact of active listening through the ImproveWell solution on teams and organisations across the UK and internationally.
Rosebrook Psychiatric Intensive Care Unit, Southern Health and Social Care Trust
Tackling culture and staff turnover: The Rosebrook Psychiatric Intensive Care Unit (PICU), Southern Health and Social Care Trust had a significant problem with staff retention and culture. The department adopted the ImproveWell solution to address these issues.
A year after launch, 100% of staff surveyed agree that ImproveWell gives them a voice and has led to a positive change in their working environment, and staff turnover has reduced by 89%.
“Whilst before we were haemorrhaging staff, in the last 12 months we haven’t lost a single staff member. And recruitment has been successful. There’s a change in how others perceive our team and it’s a place where people want to come to work. That’s a clear sign that our aim of improving culture on the ward is working,”
Leigh Ferris, Deputy Charge Nurse, Rosebrook Psychiatric Intensive Care Unit, Southern Health and Social Care Trust
Burns Service, Chelsea and Westminster Hospital NHS Foundation Trust
Giving staff the agency to make change: The Burns Service, Chelsea and Westminster Hospital NHS Foundation Trust adopted the ImproveWell solution to engage staff in creating and supporting change. Burns Matron Nicole Lee had used the ImproveWell solution during her time at the NHS Nightingale Hospital, London, and had witnessed the power of creating a 24/7 feedback loop for continuous learning and improvement.
Within 12 months of implementing ImproveWell, the Burns Service saw significant improvement both in the number of staff who feel they can easily share ideas (from 57% to 91%) and those who feel their ideas were listened to (from 57% to 72%).
“ImproveWell is part and parcel of my leadership and management style – it’s a tool that helps me to manage and engage with my staff and gives me real-time feedback on how staff are feeling. It’s easy to use and saves me hours.”
Nicole Lee, Burns Matron, Burns Service, Chelsea and Westminster Hospital NHS Foundation Trust
‘Enjoying Work’
East London NHS Foundation Trust & Royal College of Psychiatrists
Scaling up Joy in Work: East London NHS Foundation Trust adopted the ImproveWell solution to support its Enjoying Work programme in 2018. The programme sees teams applying quality improvement (QI) techniques to improve staff experience and joy, applying the Institute for Healthcare Improvement Framework for Joy in Work. Following the success at a Trust level, the Royal College of Psychiatrists launched a national Enjoying Work collaborative using ImproveWell. This 12-month collaborative provided opportunities for 38 healthcare teams across 16 UK healthcare organisations to understand and test ideas on the factors contributing to joy in work and wellbeing. Subsequently, the Institute for Healthcare Improvement launched a 12-month international Joy in Work collaborative making the ImproveWell solution available to 15 participating organisations across the NHS, US, Canada and Kenya.
Over 50 teams have gone through the ‘Enjoying Work’ programme’, underpinned by ImproveWell at East London NHS Foundation Trust. Of 21 teams in the first two cohorts, 14 demonstrated sustained improvement in the proportion of staff who felt they had a good day at work.
The 38 teams who took part in the Royal College of Psychiatrists Enjoying Work demonstrated: a 51% improvement in the percentage of people who have enjoyed being at work frequently; a 41% improvement in the percentage of people who are experiencing no symptoms of burnout; and a 42% improvement in the percentage of people who are extremely likely to recommend their team as a place to work.
“At a time when the prevailing rhetoric is about poor morale and burnout… 38 teams have shown we can improve joy and wellbeing, whilst reducing burnout, through a very simple, but powerful approach.”
Dr Amar Shah, Chief Quality Officer, ELFT and National Improvement Lead, Royal College of Psychiatrists.
Orthopaedic Surgery, M Health Fairview, University of Minnesota
Building a culture of innovation: in 2017, the Department of Orthopedic Surgery at M Health Fairview implemented the ImproveWell solution to improve staff engagement and help build a culture of innovation.
Two years post implementation, 91% of respondents felt encouraged to be innovative in finding more effective ways of doing something, compared to 67% in 2017. In addition, 82% of respondents believed their departments used innovative approaches to improving internal effectiveness, compared to 65% in 2017.
“Having this solution-based mindset empowers employees to get involved and participate in quality improvement. Our teams feel like their voice matters, like their leaders want to know what can be solved… When people are connected to others at work it builds retention – when people like who they work with they don’t want to go…”
Joy Harken, Department of Orthopaedic Surgery, University of Minnesota
*M Health Fairview is an integrated academic health system partnership between the University of Minnesota, the University of Minnesota Physicians and Fairview hospitals and clinics based in Minnesota, USA.
